Introduction
Sinusoidal obstruction syndrome (SOS), also called hepatic veno-occlusive disease (VOD) is a condition causing damage of hepatic vascular endothelial cells, it can progress to multi-organ failure and is associated with high mortality ( >80%). It is known to occur mainly after high dose chemotherapy use in hematopoietic stem cell transplant (HSCT) but with recent advances in chemotherapy, there is an increase in its incidence in non-hematopoietic stem cell transplant patients (non-HSCT). Currently, there is limited literature comparing the patient characteristics and survival of SOS in HSCT vs non-HSCT patients. Therefore we conducted this retrospective analysis.
Methods
We performed a retrospective analysis using the 2016-2020 National inpatient sample (NIS) database, generated by the Health care cost and utilization project (HCUP). We gathered data on all patients who had SOS/VOD during this time period. They were divided into two cohorts, those who received hematopoietic stem cell transplant (HSCT group) vs those who did not receive hematopoietic stem cell transplant (non-HSCT group). Among the two cohorts we compared the patients characteristics, underlying malignancies, comorbidities and mortality.
Results
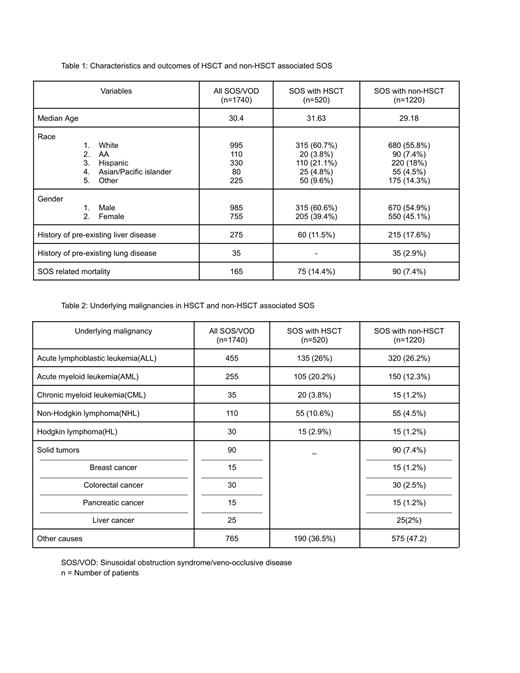
From the NIS database during the study period 1740 cases had documented SOS/VOD. Of those, 520(30%) had a history of HSCT and 1220(70%) did not have HSCT. Of the 520 cases with HSCT, 135 (26%) had Acute lymphoblastic leukemia (ALL), 105 (20.2%) had Acute myeloid leukemia (AML), 55 (10.6%) had Non-Hodgkin lymphoma (NHL), 20 (3.8%) had Chronic myeloid leukemia (CML), 15 (2.9%) had Hodgkin lymphoma (HL), the rest were other malignancies which were not included in the search. Of the 1220 cases without HSCT, 320 (26.2%) had ALL, 150 (12.3%) had AML, 90 (7.4%) had Solid tumors, 55 (4.5%) had NHL, 15 (1.2%) had CML, 15 (1.2%) had HL, the rest were likely malignancies not included in the search. ALL was the predominant cancer in both HSCT and non-HSCT groups (26% and 26.2% respectively), followed by AML, with more AMLs noted in the HSCT group (20%) versus the non-HSCT group (12.3%). The study population predominantly consisted of Whites followed by Hispanics and then African-Americans in both groups. The population also consisted predominantly of males across both cohorts. (Table 1). The solid tumors which were associated with SOS in the non-HSCT group included colorectal cancer, liver cancer, pancreatic cancer and Breast cancer in that order (Table 2). Preexisting liver disease was present in 215 (17.6%) of patients in non-HSCT cohort vs 60 (11.5%) patients in SCT cohort. Pre-existing lung disease was insignificant in both groups. Mortality was compared between the two groups after adjusting for primary cancer, age, sex, race and we found that SCT group had higher odds of mortality compared to non-SCT (14.4% vs 7.4%, aOR 1.866, 95% CI 1.29-2.68, p<0.01). Further multivariate analysis could not be carried out due to low sample size.
Discussion
Although traditionally, SOS/VOD has been thought to be a complication related to SCT, our study goes on to show that there is actually a higher incidence of SOS in the non-SCT patient population. ALL was the most common hematological malignancy encountered and had similar prevalence in both groups indicating that treatment regimens used in this cancer carry a high risk of SOS. Drugs like inotuzumab ozogamicin are the possible culprits although this information could not be obtained from our database. AML patients also exhibited high rates of SOS, more so in the SCT setting. Patients with preexisting liver disease and hematological malignancies could also benefit from close monitoring for symptoms of SOS with a high index of suspicion based on our results.
Despite rising incidence in non-SCT patients, SCT patients with SOS continue to have a higher mortality possibly indicating the higher toxicity of chemotherapy regimens used in this setting. Thus, our study brings forth some important differences between HSCT and non-HSCT SOS and enables clinicians to identify the associated risk factors.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal